What does it mean to have "pre-diabetes?" Does such a condition really exist?
In order to best understand the concept of “pre-diabetes,” it is important to understand what diabetes is.
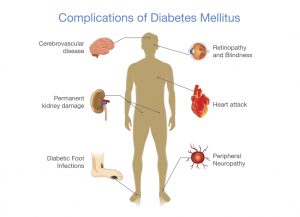
Diabetes is a condition of abnormally high blood sugar (also called blood glucose), that could cause micro-vascular complications, such as blindness and kidney failure. A diagnosis of diabetes is made when either the pancreas is not making insulin (Type 1 diabetes) or when the body’s cells have become resistant to insulin (Type 2 diabetes).
Insulin helps the body’s cells absorb glucose for energy. When the pancreas (the organ in which insulin is made) is not making insulin, glucose cannot be absorbed into the body’s cells.
Glucose, therefore, remains in the bloodstream at abnormally high levels. This condition is referred to as Type 1 diabetes, and is usually the result of an immune system response which has injured the insulin-making cells of the pancreas.
Type 1 diabetes can be managed, with a combination of daily insulin injections, diet, and exercise, but it cannot be cured.
Type 2 diabetes is diagnosed when blood glucose levels are high even though the pancreas is making insulin. With type 2 diabetes, the body becomes unable to use insulin well, as the body’s cells are unable to absorb glucose from the bloodstream efficiently.
When glucose cannot be absorbed by the cells, it remains in the bloodstream at elevated levels. Elevated levels of blood glucose stimulate more insulin production in the pancreas, until, ultimately, the pancreas cannot make enough insulin.
Diabetes type 1 and type 2 are very different; the prevention and treatment of each type of diabetes is different. With either type of diabetes, the treatment goal is to maintain normal levels of blood glucose in an attempt to avoid complications that result from chronically elevated levels of glucose, such as blindness, heart attack, stroke, kidney failure and foot problems (micro-vascular complications).
The diagnosis of “pre-diabetes” is, theoretically, a precursor to type 2 diabetes. “Pre-diabetes” indicates a degree of insulin resistance. In “pre-diabetes” blood glucose levels are not high enough to make a diagnosis of diabetes, but not low enough to be considered “normal.”
However, not everyone who is diagnosed with “pre-diabetes” will go on to develop type 2 diabetes, despite what the name implies. Not everyone who is diagnosed with “pre-diabetes” will realize an increased risk of diabetes related micro-vascular complications.
There are three different blood glucose measurements used to diagnosed diabetic conditions:
The fasting glucose level is perhaps the most accurate diagnostic test for diabetes.
The 2-hour glucose tolerance test evaluates the body’s response to 75mg of glucose, which is administered as a drink. Two hours after the drink is consumed, blood glucose is tested.
Hemoglobin A1C (also known as HgbA1C, or glycosylated hemoglobin) can be measured without any special preparation. Neither fasting nor a glucose load is required.
Hemoglobin A1C can be altered by various medical conditions, causing both over- and under- diagnosis of diabetes. Though hemoglobin A1C has been used to diagnose “pre-diabetes,” there is no evidence to support that the above noted levels indicate any degree of insulin resistance.
There is not perfect agreement among health care professionals, professional organizations, or advocacy organizations such as the American Diabetes Association on how “pre-diabetes” should be defined, diagnosed, monitored or treated.
Clarifying a definition of “pre-diabetes,” and the interpretation of the lab work in order to make a diagnosis of “pre-diabetes” are not the only concerns.
“Pre-diabetes” is likely a unique condition for some individuals, but may be too broad to warrant the concern it generates on a widespread basis. Still, attention to the prevention of diabetes and diabetic complications is justified.
 Eat a healthy diet, full of fresh vegetables and fruits, whole grains and lean protein
Eat a healthy diet, full of fresh vegetables and fruits, whole grains and lean protein

Guest Author
Carina Ryder
Certified Nurse-Midwife with 20 years of clinical experience
